Only a doctor can make a DMD diagnosis. There are a specific set of steps the doctor will go through that will help them tell whether a patient has DMD.
Doctors will look at:
Your doctor may also talk to or consult with a specialist, to confirm their decision.
Often, it’s a parent or other adult that brings the signs and symptoms of DMD to a doctor’s attention.
Keep reading to learn more about the signs of DMD in children.
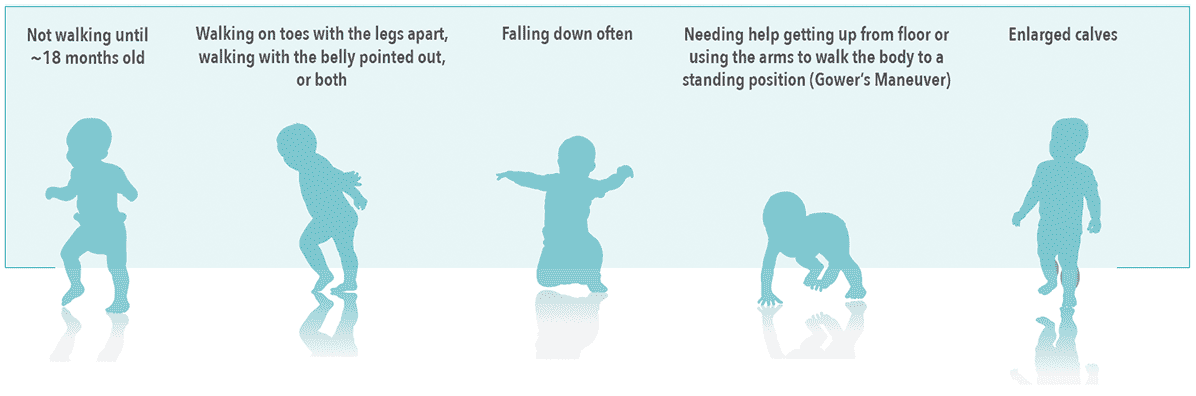
Knowing the signs and symptoms of DMD can help catch the disease early and help an affected child get the help they need.

Recognizing red flag signs and symptoms:
Take these three steps to prepare for the doctor’s visit and help them determine whether it is DMD or another condition;

Understanding your family’s history of muscle disease and other conditions can help your doctor reach a diagnosis.


Bring photos or videos to help your doctor gain a better understanding of the signs and symptoms you have observed.
The earlier a doctor makes a diagnosis, the sooner a child with DMD can start getting medical care and treatment. Getting care early gives doctors the best chance of slowing down the disease and helping to preserve muscle function for as long as possible.

If Duchenne muscular dystrophy (DMD) is suspected, the first thing your family doctor will do is perform a physical exam to check for muscle weakness. They will also ask about delays in early developmental milestones, such as sitting, walking, and standing up from the floor.

Your doctor will usually recommend a special blood test called a creatine kinase (CK) test. This involves taking a small sample of blood, which will be sent to a lab for analysis. If your child or young person has high CK levels, another sample of blood may be taken to test for changes in genes (called mutations) that cause DMD.
If your doctor becomes concerned that your child or young person needs further testing, they will usually refer them to a neuromuscular specialist. The specialist will then work to identify the cause of the symptoms and may recommend genetic testing.

Genetic testing is the only way to confirm a DMD diagnosis. It can also identify the specific genetic cause of the individual’s DMD to help narrow down treatment options, qualify a patient to participate in a clinical trial and check whether an individual is a Duchenne gene carrier, so appropriate steps can be taken.

A CK test checks for an enzyme called creatine kinase, or CK. When muscle fibers are damaged, CK leaks out into the bloodstream. The muscle damage caused by DMD means that the level of CK in the blood will often be higher than normal.
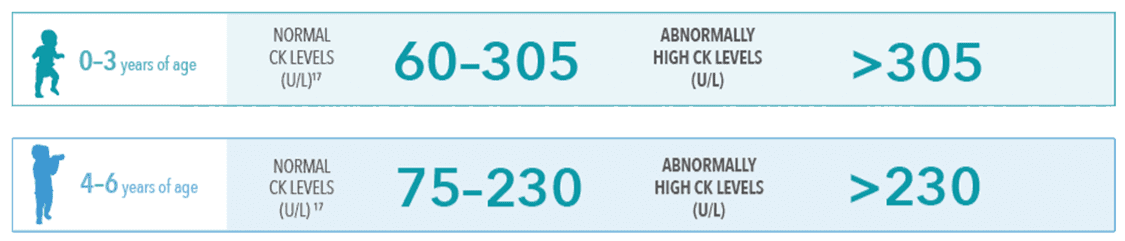
High CK levels in the blood do not automatically mean that your child or young person has DMD. Genetic testing is the only way to confirm a DMD diagnosis.
Decode Duchenne provides no-cost genetic testing, interpretation, and counseling through PPMD and PerkinElmer.

Detect MD provides no-cost genetic testing, interpretation, and counseling through Invitae.
Resources and therapies are available to help manage symptoms and possibly slow down the progression of the condition.
Your doctor will do more investigations into what else could be causing symptoms.
Different genetic tests can also tell your doctor about the type of mutation your child or young person has.This is important because different resources and therapies are available to manage different mutations.
Genetic counselors are professionals who can help guide you through genetic tests and explain how the results might affect you or your family. They also provide you with emotional support and the resources to help you cope in the long term.


They will answer any questions you have about Duchenne muscular dystrophy (DMD) and what it means for your family.
They will help determine the best testing strategy for your child or relative.

They will help you make sense of the results and discuss the best course of action.

They will help you and your family cope with a positive test result.
Deciding whether to talk to your family members about a genetic diagnosis is a very personal decision.
But you are not alone—your counselor can help you make many key decisions.
A genetic counselor can help you:
Prenatal tests can be carried out during pregnancy to try to find out whether the developing baby is affected by Duchenne muscular dystrophy (DMD).
If you have a child or relative with DMD, you may be eligible for prenatal diagnoses in future pregnancies. Once you have the results, you can talk with a genetic counselor about what the results mean for your family. To find out more about prenatal testing and whether or not you are eligible, speak to your doctor.
You can learn more about genetic testing for DMD at Decoding Duchenne– a testing program run by Parent Project Muscular Dystrophy.
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
Lurio JG, et al. Am Fam Physician. 2015;91:38–44.
Guide for primary care providers. National Task Force for Early Identification of Childhood Neuromuscular Disorde https://childmuscleweakness.org/wp-content/uploads/2019/05/PrimaryCareProviderPacket.pdf. Accessed March 2021.
Mah JK. Neuropsychiatr Dis Treat. 2016;12:1795–1807.
Guide for primary care providers. National Task Force for Early Identification of Childhood Neuromuscular Disordehttps://www.mda.org/sites/default/files/2020/10/MDA_DMD_Fact_Sheet_Oct_2020.pdf. Accessed March 2021.
Mah JK. Neuropsychiatr Dis Treat. 2016;12:1795–1807.
Aartsma-Rus A, et al. J Pediatr. 2019;204:305–313.e4.
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Patient and parent stories. Duchenne UK. Available at https://www.duchenneuk.org/Pages/Category/parent-stories. Accessed March 2021.
Assistance fund opens program to help Duchenne patients with medical expenses. Muscular Dystrophy News https://musculardystrophynews.com/10/28/assistance-fund-offers-duchenne-muscular-dystrophy-patients-help-with-medical-expenses/. Accessed March 2021.
Aartsma-Rus A, et al. J Pediatr. 2019;204:305–313.e4.
Aartsma-Rus A, et al. J Med Genet. 2016;53:145-151.
Andropoulos DB. Appendix B: Pediatric normal laboratory values. In: Gregory GA, Andropoulos DB, eds. Gregory’s Pediatric Anesthesia. 5th ed. Wiley Online Library. Accessed on September 28, 2021.https://onlinelibrary.wiley.com/doi/ abs/10.1002/9781444345186.app2
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Ciafaloni E, et al. J Pediatr. 2009;155:380-385.
Lurio JG, et al. Am Fam Physician. 2015;91:38-44.
Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
Bianco B, et al. Einstein (Sao Paulo). 2017;15:489–491.
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Helderman-van den Enden ATJM, et al. Clin Genet. 2011;79:236–242.
Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, et al., editors. Assessing genetic risks: implications for health and social policy. Washington, DC: National Academies Press (US); 1994: 4. Issues in genetic counseling. Available at https://www.ncbi.nlm.nih.gov/books/NBK236049/ [last accessed March 2021].
Parent Project Muscular Dystrophy. Genetic counseling. Available at https://www.parentprojectmd.org/about-duchenne/is-it-duchenne/genetic-counseling/ [last accessed March 2021].
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
Lurio JG, et al. Am Fam Physician. 2015;91:38–44.
Guide for primary care providers. National Task Force for Early Identification of Childhood Neuromuscular Disorde https://childmuscleweakness.org/wp-content/uploads/2019/05/PrimaryCareProviderPacket.pdf. Accessed March 2021.
Mah JK. Neuropsychiatr Dis Treat. 2016;12:1795–1807.
Guide for primary care providers. National Task Force for Early Identification of Childhood Neuromuscular Disordehttps://www.mda.org/sites/default/files/2020/10/MDA_DMD_Fact_Sheet_Oct_2020.pdf. Accessed March 2021.
Mah JK. Neuropsychiatr Dis Treat. 2016;12:1795–1807.
Aartsma-Rus A, et al. J Pediatr. 2019;204:305–313.e4.
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Patient and parent stories. Duchenne UK. Available at https://www.duchenneuk.org/Pages/Category/parent-stories. Accessed March 2021.
Assistance fund opens program to help Duchenne patients with medical expenses. Muscular Dystrophy News https://musculardystrophynews.com/10/28/assistance-fund-offers-duchenne-muscular-dystrophy-patients-help-with-medical-expenses/. Accessed March 2021.
Aartsma-Rus A, et al. J Pediatr. 2019;204:305–313.e4.
Aartsma-Rus A, et al. J Med Genet. 2016;53:145-151.
Andropoulos DB. Appendix B: Pediatric normal laboratory values. In: Gregory GA, Andropoulos DB, eds. Gregory’s Pediatric Anesthesia. 5th ed. Wiley Online Library. Accessed on September 28, 2021.https://onlinelibrary.wiley.com/doi/ abs/10.1002/9781444345186.app2
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Ciafaloni E, et al. J Pediatr. 2009;155:380-385.
Lurio JG, et al. Am Fam Physician. 2015;91:38-44.
Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
Bianco B, et al. Einstein (Sao Paulo). 2017;15:489–491.
Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267 [Part 1].
Helderman-van den Enden ATJM, et al. Clin Genet. 2011;79:236–242.
Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, et al., editors. Assessing genetic risks: implications for health and social policy. Washington, DC: National Academies Press (US); 1994: 4. Issues in genetic counseling. Available at https://www.ncbi.nlm.nih.gov/books/NBK236049/ [last accessed March 2021].
Parent Project Muscular Dystrophy. Genetic counseling. Available at https://www.parentprojectmd.org/about-duchenne/is-it-duchenne/genetic-counseling/ [last accessed March 2021].
You are about to view a website that PTC Therapeutics has not reviewed for accuracy, relevance or completeness.
PTC Therapeutics does not endorse organizations that sponsor linked external websites, products, or services that such organizations may offer; and does not control or guarantee the currency, accuracy, relevance or completeness of the information found on the linked external sites.
All trademarks includes herein are the property of their respective owners.
Sign up to receive the latest information from the Duchenne muscular dystrophy community. Be the first to receive:
News alerts
Content updates
Latest resources
Ongoing support

This site is intended for US residents only.
The information on this site is not intended to make a diagnosis or to take the place of talking to a US health care professional.
PTC Cares™ is a trademark of PTC Therapeutics.
© 2022 PTC Therapeutics, Inc. All rights reserved.
Date of preparation: September 2022
MAT-CORP-0268
Neuromuscular disorders affect the muscles and nerves, and most of the causes are genetic. This means they are either passed down through the family or caused by changes in an individual person’s genes.
Most neuromuscular disorders cause muscle weakness that worsens over time. Signs and symptoms of neuromuscular diseases can vary and may be mild, moderate, or severe.
Most often, when a child has a neuromuscular disease, they don’t grow and develop as fast as other children their age. They are often slow to start lifting their head, sitting, walking, and talking.
Treatment and supportive care may improve the symptoms of a neuromuscular disorder, increasing mobility and even life expectancy.
Muscular dystrophy is the term for a group of neuromuscular disorders that cause muscle weakness and muscle loss.
Duchenne muscular dystrophy (DMD) is a type of muscular dystrophy that causes muscle weakness that worsens over time. The progression and symptoms can vary from person to person.