Living with Duchenne Muscular Dystrophy (DMD)
_
Overview
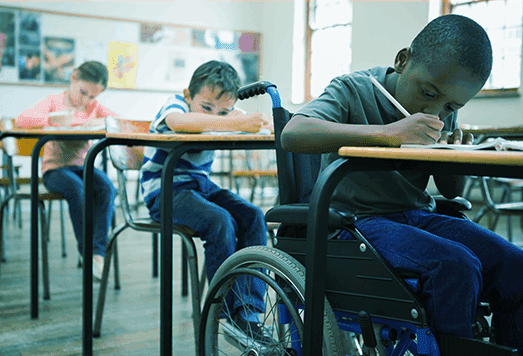
A DMD diagnosis is devastating—but it doesn’t have to defeat you or your child.
People live productive, creative, and fulfilling lives with DMD.
More and more young adults with DMD are attending university, pursuing rewarding careers and even having families of their own.
To help your child make the most of their future, start by finding out what adaptations can be made to enable them to participate in school as fully as possible. They deserve the same access to learning as any other child.
Then, connect with other people who are going through DMD. Talking to others about having DMD can be daunting, in this section we also provide you with some tips on deciding who to tell, where to start, how to explain what it is like to live with DMD, answering questions, and importantly, responding to people’s reactions.
Read more below—we hope it helps you build a better life with DMD.
What to expect from DMD
The symptoms of DMD are different for each child and the rate at which symptoms worsen varies. And, as time goes on, the symptoms of DMD will change:
- As the muscles get weaker, the ability to walk is slowly lost
- As the back muscles become weaker, the spine may begin to curve (called scoliosis)
- In late childhood to early adulthood, the upper body and arm muscles also weaken
- The heart and respiratory (or breathing) muscles also weaken over time, which can lead to complications
As DMD is a progressive disease, meaning the symptoms become more apparent over time, it is important to get your child the right treatments and management as soon as possible. This gives your child the best chance of maintaining their independence and quality of life for as long as possible.